Medicaid typically covers medically necessary surgeries that treat an illness or injury or correct a functional impairment.
Meanwhile, Medicaid and other insurance programs deem abdominoplasty cosmetic as it improves one’s appearance, and the medical benefits are unproven.
Even if you have back pain, urinary incontinence, or a ventral hernia, your Managed Care Organization (MCO) is unlikely to pay a tummy tuck claim.
However, a partial victory remains possible: reduce costs by combining abdominoplasty with a medically necessary procedure Medicaid does cover. Then, find a local doctor who accepts your Medicaid plan and convince the plastic surgeon to perform two operations simultaneously.
Medicaid Covering Tummy Tucks
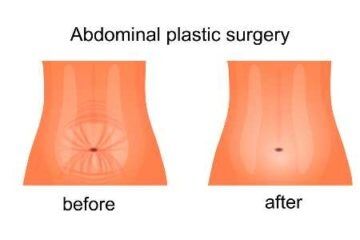
You must overcome one enormous obstacle to get Medicaid to cover a tummy tuck. Abdominoplasty is cosmetic and not medically necessary when removing excess skin or fat with or without tightening the underlying muscles.
Tummy tuck financing with poor credit might be a better avenue toward a trimmer waistline. Medicaid is unlikely to pay any cost for this procedure unless it is performed simultaneously with another medically necessary operation. Below are several possibilities.
After Weight Loss
If combined with another medically necessary procedure, Medicaid might cover some of your tummy tuck costs after significant weight loss. You might save money on the anesthesia, nurses, operating room, and other shared expenses.
Medicaid often covers Panniculectomy after weight loss surgery when the excess skin hangs below the symphysis pubis (joint between two pubic bones), causing a functional impairment that has not responded to less invasive treatments.
After C-Section
If combined with another medically necessary procedure, Medicaid might cover some of your tummy tuck costs after a C-section. Doctors strongly advise women to wait until they finish having babies before undergoing abdominoplasty.
Medicaid often covers tubal ligation (not reversal) as a permanent contraception method. Schedule both procedures on the same day, months after your last Cesarean section, to save money on anesthesia, nurses, operating room, and other shared expenses.
With Liposuction
Medicaid might cover some of your tummy tuck costs if combined with a medically necessary Liposuction, saving you money on the anesthesia, nurses, operating room, and other shared expenses.
Medicaid often pays for Liposuction if you can establish a medically necessary reason to harvest fast from targeted areas on your body. Two conditions often qualify.
- Treat lipedema (abnormal build-up of fat in your legs and arms, causing pain or limiting movement)
- Support breast reconstruction after mastectomy or lumpectomy requiring the harvesting and grafting of autologous fat
With Hernia Repair
Medicaid might cover some of your tummy tuck costs if combined with a medically necessary hernia repair, saving you money on the anesthesia, nurses, operating room, and other shared expenses.
Apply for temporary disability after hernia surgery and possibly save even more money by replacing a portion of your income while you recover.
A hernia occurs when part of your abdominal organs bulges through an opening or weakness in the muscle or tissue that contains it. If not treated, necrosis (tissue death) can occur.
With Hysterectomy
Medicaid might cover a portion of your tummy tuck costs if combined with a medically necessary hysterectomy (removal of the uterus). Hysterectomies are needed when a patient has abnormal bleeding, pain in the pelvic region, endometriosis, cancer, or uterine fibroids.
Studies show hysterectomies and abdominoplasties can be performed simultaneously, possibly saving you money on anesthesia, nurses, operating room, and other shared expenses. Discuss the pros and cons with your gynecologist before proceeding.
Doctors Accepting Medicaid
Another consideration is looking for local plastic surgeons who accept Medicaid for tummy tucks, provided you need a second medically necessary procedure. If your motivation is purely cosmetic, no doctor will take your coverage, regardless of their affiliations.
Provider Directory
The online provider directory published by your Managed Care Organization (MCO) or state agency is the primary way to find a surgeon who takes Medicaid for tummy tucks.
Each state contracts with different MCOs to administer its plans. Open your wallet and retrieve your membership card to find the correct entity. Then, go to the designated website and find the provider directory.
- Input your zip code
- Select plastic surgery for specialty
- Get a listing of local participating providers
Of course, besides finding a doctor who takes your Medicaid plan administered by your specific MCO, you must convince the surgeon to perform two procedures simultaneously.
Primary Provider
Your primary care provider (PCP) is sometimes the only avenue to find a local doctor who accepts your Medicaid plan for tummy tucks. Many recipients enroll in Health Maintenance Organizations (HMOs) that require specialist referrals.
For example, many Medi-Cal programs operate under this model.
Therefore, your first step is meeting with your designated PCP, who must diagnose you with a problematic pannus, lipedema, uterus, or hernia or recognize the need for breast reconstruction after a mastectomy. The primary care doctor would then refer you to a nearby plastic surgeon who would participate in your HMO-like treatment plan.